Neurology
Alzheimer's Disease
Evolution in Thinking About Amyloid in Alzheimer’s Disease
I do not think that we should use the term “amyloid hypothesis” in the context of Alzheimer’s disease, since the use of “hypothesis” nowadays is pejorative. I no longer consider amyloid a hypothesis, but a target. Amyloid is a toxic degradation product that accumulates in the brains of patients with Alzheimer’s disease. We think that these species of breakdown products begin accumulating long before clinical symptoms develop, maybe 20 years in advance, and, over time, manifest themselves as clinical disease. We know that amyloid can accumulate while we are unaware that it is happening.
We hoped for a very long time that by removing the amyloid we would also be slowing the progression of the disease and making a beneficial difference in terms of cognition and functional activities compared with the effects seen in patients who do not receive an amyloid-targeted therapy. Amyloid is now an accessible target, and we have 2 FDA-approved amyloid-targeted therapies (ie, donanemab with full approval and lecanemab with accelerated approval) that help slow the progression of Alzheimer’s disease in patients with the mild cognitive impairment of Alzheimer’s disease. These monoclonal antibodies, in one way or another, remove parts of different amyloid moieties. We are trying to interrupt what is going on as soon as we detect disease.
Although it is very exciting to have 2 FDA-approved targeted therapies for amyloid, we are all energized now because we have the opportunity to look at other targets that show promise. One target that is currently being pursued is tau, which, like amyloid, is a breakdown product. In fact, while there are separate mechanisms involved in their development and clearance, amyloid and tau are intimately related.
Many people who were enrolled in the clinical trials for the FDA-approved amyloid-targeting therapies were also receiving symptomatic treatment with acetylcholinesterase inhibitors. This lends credence to the idea that Alzheimer’s disease treatment is going to be a cocktail of drugs.
We now know that the overaccumulation or an underclearance of amyloid is the earliest seminal event in Alzheimer’s disease, and everything downstream occurs because of that. Without amyloid, you do not have Alzheimer’s disease. You may have another neurodegenerative disease or other degradation of the brain, but it is not Alzheimer’s disease.
We also now know that only once amyloid starts to accumulate into the oligomeric species does the brain say, “Oh, that’s not supposed to be here.” That is when you get microglia activation, an inflammatory response, the triggering and spread of the tau, and everything else that happens downstream of amyloid accumulation.
I agree very much with Dr Tangalos that we are no longer talking about a hypothesis with amyloid, but rather a mechanism or drug target. I think that the future of Alzheimer’s disease treatment is going to be a multidrug chemotherapy-style cocktail in which we target amyloid, tau, inflammation, and neurochemical changes. It is going to be something we have to do with a combination of therapies. But I think that the result would be that we could arrest the clinical progression of Alzheimer’s disease.
I really like the concept of moving away from referring to amyloid as a hypothesis to calling it a target. Something that really needs to be heard is that prior to cognitive change, there are structural brain changes that start with amyloid decades before the onset of symptoms. When these changes in the brain start to occur, patients are often in their 40s and 50s, and when patients that age see me in primary care, I offer advice about maintaining healthy lifestyles, body weight, and good sleep habits; and staying mentally and physically active. I think that primary care physicians should understand that we are fighting not only the onset of diabetes and cardiovascular disease in patients in this age group but also cognitive decline.
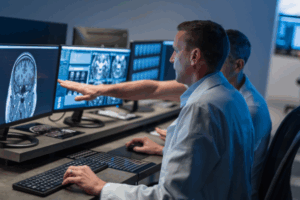
When primary care physicians identify somebody with any kind of symptom or concern regarding cognitive decline, it is our job to screen those individuals and initiate a workup, which includes a basic laboratory workup and magnetic resonance imaging of the brain.
Chen Y, Yu Y. Tau and neuroinflammation in Alzheimer’s disease: interplay mechanisms and clinical translation. J Neuroinflammation. 2023;20(1):165. doi:10.1186/s12974-023-02853-3
Congdon EE, Ji C, Tetlow AM, Jiang Y, Sigurdsson EM. Tau-targeting therapies for Alzheimer disease: current status and future directions. Nat Rev Neurol. 2023;19(12):715-736. doi:10.1038/s41582-023-00883-2
Kepp KP, Robakis NK, Høilund-Carlsen PF, Sensi SL, Vissel B. The amyloid cascade hypothesis: an updated critical review. Brain. 2023;146(10):3969-3990. doi:10.1093/brain/awad159
Wang Q, Xie C. Microglia activation linking amyloid-β drive tau spatial propagation in Alzheimer’s disease. Front Neurosci. 2022;16:951128. doi:10.3389/fnins.2022.951128
Wu W, Ji Y, Wang Z, et al. The FDA-approved anti-amyloid-β monoclonal antibodies for the treatment of Alzheimer’s disease: a systematic review and meta-analysis of randomized controlled trials. Eur J Med Res. 2023;28(1):544. doi:10.1186/s40001-023-01512-w